Release date:2023-04-07
Creatine kinase (CK) is one of the important diagnostic enzyme markers in human blood, widely distributed in skeletal muscles, myocardium, gastrointestinal tract, brain tissue, etc.
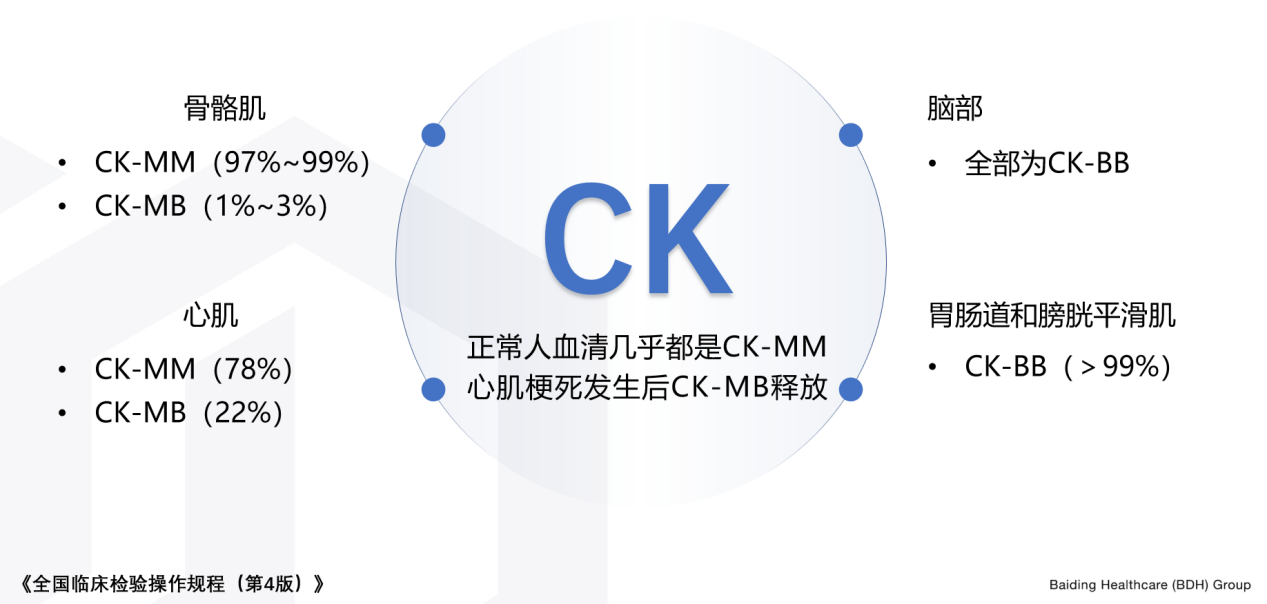
CK is a dimeric structure, including M and B subunits, so there are three isoenzymes: CK-MM, CK-MB, and CK-BB. The distribution of CK in different tissues is shown in the figure below.
In addition, there is also a mitochondrial CK. In rare cases, there are two types of giant CK in serum, namely, giant CK1, which is a complex of CK with immunoglobulin, and giant CK2, which is a mitochondrial CK polymer.
Among CK isoenzymes, CK-MB mainly exists in cardiomyocytes and has good myocardial specificity. In clinical practice, in addition to cardiac troponin, CK-MB is still the main marker of myocardial injury.

I. Methodology of CK-MB Biochemical Detection Platform
CK-MB is a routine detection item in the biochemical detection platform, and the main detection method in the past was the immunosuppression method.
Under normal circumstances, almost all CK in the peripheral blood circulation of humans is CK-MM isoenzyme. In the case of myocardial injury, such as acute myocardial infarction (AMI), cardiomyocytes release CK-MB isoenzyme into the blood. The principle of the immunosuppression method is to inhibit the activity of the M subunit in the specimen with anti-M subunit antibody, and then use CK assay reagents to determine the activity of the B subunit to calculate the activity of CK-MB. The results detected by this method may actually be the activities of CK-MB and CK-BB, but since the content of CK-BB in the blood is usually very low, it can reflect the activity of CK-MB.
When the level of CK-BB in the blood is abnormally elevated or giant CK1 and giant CK2 are present, it can lead to abnormally elevated results of CK-MB detected by the immunosuppression method, exceeding the true activity of CK-MB, and even exceeding the total CK activity. This situation is called the phenomenon of result inversion. Under normal circumstances, the activity of CK-MB in peripheral blood samples of humans is not greater than 25 U/L, accounting for less than 3% of the total CK activity. When the total CK activity increases and the CK-MB/CK ratio activity is between 10% and 30%, there is a high risk of myocardial injury.
In recent years, mass detection of CK-MB by immunological methods has become more and more widely used in clinical applications. The latex-enhanced immunoturbidimetric method of the biochemical platform forms an immune complex with CK-MB through antibody latex particles, and then measures the content of CK-MB by turbidimetry. It has been found that the mass method of CK-MB detection can effectively avoid the interference of CK-BB and other enzymes on the results, as shown in Table 1.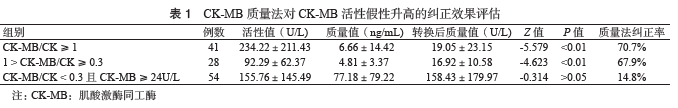
When CK-MB/CK ≥ 0.3, the mass method can effectively avoid the interference of other isoenzymes. When CK-MB ≥ 24 U/L and CK-MB/CK < 0.3, most patients are diagnosed with AMI, and the consistency between the results of the activity method and the mass method is high.

II. Selection of CK-MB Methodology
Due to its higher specificity, mass detection is more suitable for clinical application compared to the activity method.
The "WS/T 462-2015 of the People's Republic of China Health Industry Standard: Detection and Clinical Application of Heart Markers in Coronary Artery Disease and Heart Failure" proposes: "CK-MB mass determination has better analytical and diagnostic utility and is significantly better than activity determination."
Therefore, when conditions permit, it is recommended to use the latex-enhanced immunoturbidimetric method to detect CK-MB mass.

III. Clinical Application of CK-MB Mass Results
1.Diagnosis of myocardial infarction: Two consecutive positive CK-MB results indicate myocardial necrosis. Combined with electrocardiogram or other ischemic evidence, early diagnosis of myocardial infarction can be made.
2. Biomarker detection after myocardial infarction: CK-MB returns to normal within 48-72 hours, so it can rapidly differentiate reinfarction within 72 hours to 2 weeks, and it is the preferred biomarker for early detection of reinfarction after myocardial infarction. After diagnosing myocardial infarction, test three times at intervals of 6 to 18 hours to qualitatively assess infarct size and detect complications such as reinfarction.
3. Non-invasive assessment of reperfusion: The rising/falling pattern of myocardial necrosis markers can assist in reperfusion assessment; early in thrombolysis, when the blocked artery is reperfused, the markers overflow from the damaged cells, resulting in an early peak; the rate of increase in markers hours after treatment indicates the degree of reperfusion of the infarct-related artery.
4. Prognostic assessment of ACS: The CK-MB concentration at admission is positively correlated with the mortality rate at 30 days and 6 months later.
References:
[1]Zhao H, Yin XC, Zhang LC. Reasons and clinical value of result inversion in the detection of creatine kinase and its isoenzymes by immunosuppression method[J]. Agriculture and Reclamation Medicine, 2022, 44(1):4.
[2] Tian Q, Li H, Zhang Y, et al. Analysis of cases where serum creatine kinase isoenzyme activity is greater than creatine kinase[J]. International Journal of Laboratory Medicine, 2022, 43(14):4.
[3]Shen SE, Zhang HR. Performance evaluation of creatine kinase isoenzyme mass method in assisting diagnosis of myocardial infarction[J]. Cardiovascular Disease Prevention and Treatment, 2022(004):022.
[4] Alexander J H , Sparapani R A , Mahaffey K W , et al. Association Between Minor Elevations of Creatine Kinase-MB Level and Mortality in Patients With Acute Coronary Syndromes Without ST-Segment Elevation[J]. Jama, 2000, 283(3):347-353.


