Release date:2022-08-04
In 2019, the National Health Commission of China launched the "Healthy China Action (2019-2030)", which includes the "Cardiovascular and Cerebrovascular Disease Prevention and Control Action", proposing several action targets for reducing mortality, increasing awareness, and improving control rates of cardiovascular and cerebrovascular diseases. The action advocates for regular health check-ups for residents and recommends that high-risk groups undergo lipid profile testing every six months.
Traditional lipid profile testing includes triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C). Traditional lipid profile testing can reflect abnormalities in lipid metabolism, but it lacks specificity in predicting cardiovascular disease. In recent years, domestic and international cardiovascular disease-related guidelines have recommended several new lipid markers for disease risk assessment. This article mainly introduces one of these new markers, lipoprotein-associated phospholipase A2 (Lp-PLA2), which is closely related to vulnerable plaque in blood vessels.

I. What is Lp-PLA2
Lp-PLA2, also known as platelet-activating factor acetylhydrolase, is an inflammation marker with endothelial specificity in cardiovascular disease.
Lp-PLA2 is secreted by macrophages, T cells, and mast cells in the vascular endothelium. After being released into the bloodstream, 80% of Lp-PLA2 binds to LDL, with the remainder binding to HDL, Lp(a), VLDL, etc.

II. Lp-PLA2 and Atherosclerotic Diseases
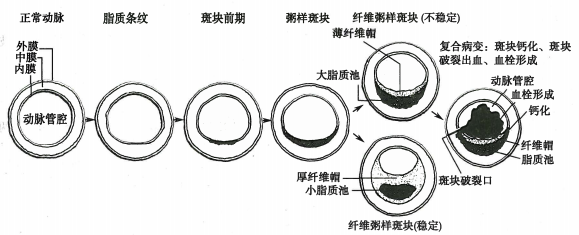
Under certain conditions, cholesterol-rich low-density lipoprotein (LDL) in the blood can penetrate into the subendothelial layer of blood vessels. Oxidized LDL (ox-LDL) in this layer cannot be recognized by LDL receptors and instead binds to scavenger receptors on the surface of macrophages, leading to foam cell formation. Arterial smooth muscle cells proliferate and migrate, forming a fibrous cap. Ox-LDL causes foam cells to necrotize and disintegrate, ultimately forming atherosclerotic plaques.
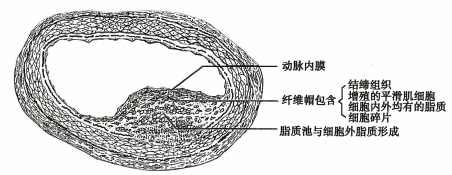
Lp-PLA2 expression is upregulated in atherosclerotic plaques. Lp-PLA2 can hydrolyze oxidized phospholipids in ox-LDL, generating lipid inflammatory mediators such as lysophosphatidylcholine and oxidized free fatty acids, which play various roles in promoting atherosclerosis and can form a self-reinforcing cycle, generating more inflammatory mediators. Therefore, Lp-PLA2 is closely related to the formation and development of atherosclerotic diseases.
The rupture or erosion of atherosclerotic plaques is the main cause of unstable angina and non-ST segment elevation myocardial infarction. ST-segment elevation myocardial infarction is usually caused by thrombus formation on the basis of rupture or erosion of unstable plaques, leading to continuous and complete occlusion of coronary arteries. Therefore, the risk of unstable plaques is higher. Lp-PLA2 is strongly expressed in macrophages in the fibrous cap of vulnerable plaques and can be used as an auxiliary indicator for assessing plaque vulnerability.
For asymptomatic high-risk individuals, the level of Lp-PLA2 can predict the risk of cardiovascular events. Studies have shown that in acute events such as acute coronary syndrome (ACS), the level of Lp-PLA2 gradually decreases after the acute phase, is significantly lower in the recovery phase than in the acute phase, and is also lower than in stable coronary heart disease. Meanwhile, as a marker of unstable atherosclerotic plaques, Lp-PLA2 can identify acute transient ischemic attacks and stroke events caused by atherosclerosis-induced stenosis of arteries. Therefore, higher levels of Lp-PLA2 generally indicate a higher risk of disease recurrence.
Various drugs can affect the level of Lp-PLA2, and statins significantly reduce Lp-PLA2 levels. There are reports that the level of Lp-PLA2 in patients treated with rosuvastatin can decrease by up to 33%.

III. Clinical Application of Lp-PLA2
The "Chinese Guidelines for Primary Prevention of Cerebrovascular Diseases" suggest that Lp-PLA2 testing can be considered for high-risk individuals of cerebrovascular disease to assess the risk of cerebrovascular events (Class III recommendation, Level B evidence);
In international guidelines for heart disease or stroke, such as those in the United States and Europe, repeated recommendations have been made to test Lp-PLA2 in high-risk or recurrent risk populations to further assess the risk of developing cardiovascular and cerebrovascular diseases.
Based on the recommendations of various guidelines, the clinical applications of Lp-PLA2 are as follows:
1. For individuals at high risk of cardiovascular and cerebrovascular diseases, including asymptomatic individuals, Lp-PLA2 testing can be added to traditional lipid profile screening to further assess the risk of developing cardiovascular and cerebrovascular diseases and more accurately identify high-risk individuals;
2. For patients already receiving statin therapy, especially those whose cholesterol levels are well controlled, measuring Lp-PLA2 levels can improve the predictive value of cardiovascular events;
3. In the case of acute thrombotic events, such as ACS and ischemic stroke, Lp-PLA2 helps in the long-term risk assessment.

IV. Methodology for Monitoring Lp-PLA2
There are two methods for detecting Lp-PLA2 in blood: activity and mass. The activity detection method uses enzymatic methods, where Lp-PLA2 breaks down substrates to produce colored products, and the activity result is obtained through continuous monitoring. The mass detection method mainly uses immunological methods, including immunoturbidimetry and chemiluminescence.
According to literature reports, both the activity and mass detection methods can meet the clinical application requirements well in terms of precision, accuracy, and measurement range. However, there are differences in the results between the two methodologies, and they have different applicable reference ranges.
References:
[1]Ge J, Xu Y. Internal Medicine [M]. People's Medical Publishing House, 2018.
[2]Bu H, Li Y. Pathology [M]. People's Medical Publishing House, 2018.
[3] Chinese Society of Geriatrics, Cardiovascular and Cerebrovascular Disease Committee. Clinical application expert consensus on lipoprotein-associated phospholipase A2 [J]. Chinese Journal of Cardiovascular Diseases, 2015(21):9-9.
[4] Chen X, Ma R, Tao S, et al. Evaluation of the consistency between serum Lp-PLA2 mass and activity detection results [J]. Laboratory Medicine and Clinical, 2019, 16(23):5.
[5]Psaty K W. Cardiovascular disease risk prediction factors: lipid-related markers and cardiovascular disease prediction [J]. JAMA, 2012, 308(19):1969-1969.
[6]Chinese Society of Neurology, Cerebrovascular Disease Group, Chinese Medical Association Neurology Branch. Chinese


