Release date:2022-06-22
Traditional blood lipid indicators include triglycerides, total cholesterol, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol, which can reflect the status of lipid metabolism in the body, identify abnormalities in lipid metabolism, and indicate disease risk.
In addition to traditional blood lipid indicators, the "Chinese Adult Dyslipidemia Prevention and Treatment Guidelines (2016 Revised Edition)" also recommend non-traditional blood lipid indicators as targets for the prevention and control of atherosclerotic cardiovascular disease (ASCVD), including non-high-density lipoprotein cholesterol (non-HDL-C) and remnant lipoprotein cholesterol (RLP).

I. Non-High-Density Lipoprotein Cholesterol
What is Non-High-Density Lipoprotein Cholesterol
Non-high-density lipoprotein cholesterol refers to the sum of cholesterol content in lipoproteins other than HDL, including all cholesterol carried by lipoproteins containing ApoB.
A large amount of evidence suggests that non-HDL-C is strongly associated with the risk of ASCVD, and the test results are stable and reliable, making it applicable for predicting the risk of ASCVD occurrence. The "Chinese Adult Dyslipidemia Prevention and Treatment Guidelines (2016 Revised Edition)" list non-HDL-C as the primary target for primary and secondary prevention of ASCVD.
Detection of Non-High-Density Lipoprotein Cholesterol
According to the definition, the content of non-HDL-C can be calculated from the results of traditional lipid tests using the following formula:
Non-HDL-C = Total Cholesterol - HDL-C
Impact of Non-High-Density Lipoprotein Cholesterol on Lipid Health
Research shows that for every 0.8 mmol/L increase in non-HDL-C, the risk of cardiovascular death increases by 19% in men and 11% in women. In people with normal LDL-C levels, when non-HDL-C exceeds 3.4 mmol/L, the risk of cardiovascular events increases by 32%. In diabetic patients, lipid metabolism abnormalities are often characterized by inconsistencies in LDL-C and non-HDL-C levels, especially in patients with high triglycerides, where non-HDL-C abnormalities are more common than LDL-C abnormalities.
Non-HDL-C, as a secondary intervention target, can be used in ASCVD risk management. The "Chinese Adult Dyslipidemia Prevention and Treatment Guidelines (2016 Revised Edition)" suggest that the ideal level of non-HDL-C is <3.4 mmol/L, with treatment target values as shown in the figure.
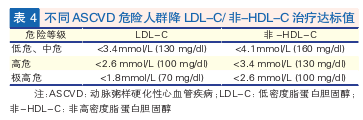
Internationally, experts in the United States recommend using LDL-C and non-HDL-C simultaneously as the primary treatment targets for primary and secondary prevention of ASCVD. The European Dyslipidemia Management Guidelines recommend using non-HDL-C as a routine test indicator for patients with diabetes and high triglycerides, obesity, and low LDL-C, as well as a secondary treatment target.
Therefore, adding non-HDL-C testing on the basis of traditional blood lipid indicators, especially for obese, high triglyceride, diabetic, or low LDL-C populations, can better predict the risk of ASCVD.

II. Remnant Lipoprotein Cholesterol
What is Remnant Lipoprotein Cholesterol
Cholesterol contained in remnant lipoproteins (RLP) is called remnant lipoprotein cholesterol, which, in the fasting state, includes cholesterol in hydrolyzed VLDL and IDL, and postprandially also includes cholesterol in chylomicron remnants (CMR-C).
CM and VLDL are lipoproteins rich in triglycerides. After hydrolysis by lipoprotein lipase (LPL), they lose triglycerides, phospholipids, apolipoprotein A, and apolipoprotein C, and are transformed into small particles rich in cholesterol, cholesterol esters, and apolipoprotein E, namely remnant lipoproteins. The remnants from the intestine are mainly composed of ApoB48 and ApoE, while those from the liver are mainly composed of ApoB100 and ApoE. Compared with triglyceride-rich lipoproteins, RLP has a stronger pro-atherosclerotic effect.
Detection of Remnant Lipoprotein Cholesterol
The "Chinese Expert Consensus on Non-Traditional Blood Lipid Indicators and Risk Management of Atherosclerotic Cardiovascular Disease" recommends using the calculation method to obtain the value of RPL-C, as the calculation method more effectively reflects the residual risk of ASCVD. The calculation formula is as follows:
RLP-C = Total Cholesterol - HDL-C - LDL-C
The consensus recommends reference ranges for healthy adults as follows:
Fasting: <0.8 mmol/L
Non-fasting: <0.9 mmol/L
Impact of Remnant Lipoprotein Cholesterol on Vascular Health
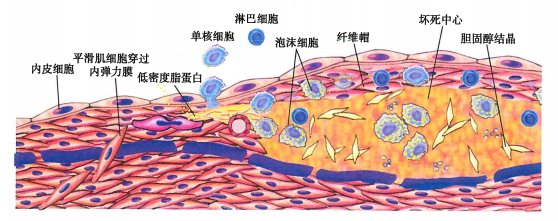
The mechanism by which elevated remnant lipoprotein cholesterol leads to atherosclerosis differs from that of LDL-C. RLP-C carries cholesterol without the need for oxidation modification. After passing through the arterial wall, it can be directly taken up and absorbed by macrophages before LDL-C by forming foam cells. Because RLP has a larger volume, its ability to carry cholesterol is 40 times that of LDL, making it more likely to form atherosclerotic plaques. It also causes local inflammation on the surface of the endothelium and at atherosclerotic sites, leading to increased endothelial permeability and further aggravating atherosclerosis.
Epidemiological studies have confirmed that RLP levels are closely related to the occurrence and development of various cerebrovascular diseases (CVD), independent of other lipids, and are also one of the residual risk markers for CVD.
The "Chinese Adult Dyslipidemia Prevention and Treatment Guidelines (2016 Revised Edition)" propose that hypertriglyceridemia often reflects an increase in remnant lipoproteins, with these particles becoming smaller and having a direct pro-atherosclerotic effect.
The Japanese Society for Atherosclerosis includes RLP-C, sd LDL-C, and Lp(a) as routine laboratory screening items for CVD prevention and risk management in its guidelines. The NCEP Adult Treatment Panel report from the United States highlights the role of RLP-C in assessing CVD risk, with highly atherogenic properties. In addition, a large number of epidemiological and genetic studies have also confirmed the role of elevated RLP-C in the development of ASCVD.
Therefore, RLP-C can provide important assistance in blood lipid management and risk control for ASCVD patients.

Summary
Elevated fasting triglycerides typically indicate an increase in chylomicrons (CM) or very low-density lipoproteins (VLDL) and remnant lipoproteins (RLP), with increased RLP directly contributing to atherosclerosis. As triglyceride (TG) levels increase, both non-high-density lipoprotein cholesterol (non-HDL-C) and RPL-C also increase, and they are positively correlated with TG. Compared to TG, non-HDL-C and RPL-C better predict the risk of atherosclerotic cardiovascular disease (ASCVD) by reflecting RLP levels.
References:
[1]Zheng Tiesheng, Yan Shengkai. Clinical Biochemical Examination. 4th Edition [M]. China Medical Science and Technology Press, 2020.
[2]Fu Weiling, Xu Keqian. Clinical Biochemical Examination [M]. People's Health Publishing House, 2012.
[3] Joint Committee for the Revision of China's Adult Blood Lipid Abnormality Prevention and Treatment Guidelines. China's Adult Blood Lipid Abnormality Prevention and Treatment Guidelines (2016 Revised Edition) [J]. Chinese Journal of Health Management, 2017, 011(001):7-28.
[4] Chinese Society of Integrated Traditional Chinese and Western Medicine Laboratory Medicine Committee. Chinese Expert Consensus on Non-traditional Blood Lipid Indexes and Atherosclerotic Cardiovascular Disease Risk Management [J]. Chinese Journal of Preventive Medicine, 2022, 56(04):405-421.
[5]Song Yunxiao, Ge Wen, Zhang Haichen, et al. Clinical value of remnant lipoprotein cholesterol in blood lipid management [J]. Laboratory Medicine, 2019, 034(005):394-400.


